Tick Bites & Lyme Disease | My Family's Story

Lyme Disease is a growing issue
throughout the world, creating a significant health crisis. If you follow me on social media, you know that I'm an advocate of organic food and natural approaches to health and wellbeing, speaking out against products that contain harmful ingredients and the companies that produce them.
When discussing Lyme Disease, it's imperative to talk about the medical reality attached to this issue. Let me state, for the record, the information that is shared here is not a substitute for medical advice or care. Please use this information at your own discretion and share it with your primary health practitioner. The information available about Lyme Disease is changing daily, so please investigate any further developments.
The following is an article written by my sister, Lynn Daniluk. As you will see she has quite a bit of personal experience dealing with Lyme. She has included resources throughout this article so that you can do your own research.
My family's experience with Lyme Disease
by Lynn Daniluk
Please note: The following is a personal story and is not meant to substitute for medical care. Please seek the help of a qualified health practitioner such as a Naturopathic Doctor or Holistic Medical Doctor that specializes in the treatment of Lyme Disease.
What is Lyme Disease?
There is no simple answer. Searching the internet, you'll discover this answer, “Lyme disease is caused by the bacterium Borrelia burgdorferi and is transmitted to humans through the bite of infected blacklegged ticks.”
Unfortunately, it's much more complicated than that.
As it turns out, Borrelia burgdorferi is only one of many bacteria that can be transmitted by these ticks; bacteria and parasites that can cause a host of infections that complicate Lyme symptoms. A patient with Lyme Disease can become infected with any combination of 28 different coinfections (at last count) including Chlamydia, Rickettsiosis, Syphillis, Anaplasma, Babesia, Mycoplasma and Ehrlichia.
Why is Lyme Disease called "Lyme Disease"?
In the early 1970s, a group of rheumatoid arthritis cases occurred among children in Lyme, Connecticut. Puzzled by the number of cases and the age of the patients, researchers looked at several possible causes, such as contact with germs (microbes) in water or air. Realizing that most of the children with arthritis lived and played near wooded areas, they began to focus their attention on deer ticks. The children’s first symptoms typically started during the summer, the height of tick season. Several children reported having a skin rash just before developing arthritis and many of them recalled being bitten by a tick where the rash appeared. (Note: we now know that the bullseye rash can appear anywhere on the body, not just in the area where a bite has occurred. Also, the rash does not appear in all cases of Lyme Disease.) In the mid-1970s, researchers began describing the signs and symptoms of this new disease, now termed Lyme Disease, to help physicians diagnose patients. However, it was not until 1981 that researchers at Rocky Mountain Laboratories in Hamilton, Montana, identified the cause of Lyme Disease making the connection between deer ticks and the disease.
What is a tick?
Ticks are small arachnids (yes, they have eight legs and are related to spiders) that are in the same subclass as mites. They can range in colour from different shades of brown to reddish-brown and black. Generally located in wooded areas, ticks can be found pretty much anywhere as birds and animals they feed on (deer!) carry them everywhere. There are about 900 species of ticks in the world (80 species living in the United States and about 40 species in Canada). It is thought that only a few species can transmit Lyme Disease; that is up for debate. According to Lyme Disease expert Stephen Harrod Buhner, the "Borrelia spirochetes are present in a variety of other biting arthropods, such as mosquitos, mites, fleas and biting flies and transmission through some of these routes has been documented." (1)
Ticks are ectoparasites, which means they live off the blood of mammals, birds and sometimes reptiles and amphibians. Ticks prefer warm, moist areas of the body so once a tick gets on your body, it is likely to migrate to your armpits, groin, genitals or scalp. When ticks find a desirable spot, they bite into your skin and begin drawing blood. Tick bites are painless; you cannot feel a tick crawl on your body, bite your skin or embed its head in your body. Unlike many other bugs that bite, ticks typically remain attached to your body after they bite you. As they draw in more blood, ticks become engorged and can grow to the size of your thumbnail. When a tick has been feeding on the host for several days or weeks, their engorged body will turn a greenish-blue colour. After several days or weeks of drawing blood, an engorged tick can detach itself and fall off.
Symptoms of Lyme Disease and how to diagnose it
Your doctor may have a difficult time diagnosing Lyme Disease as many of the symptoms are similar to other illnesses, such as the flu. You may or may not experience a combination of the following: a high temperature, aches, chills, disorientation, nausea, vomiting, migraine, joint pain, light sensitivity, lack of coordination, vertigo, stiff neck and fatigue. The bullseye rash is the only symptom that is unique to Lyme Disease, though not everyone infected with the Lyme bacteria develops the rash. Conversely, you can also have the bullseye rash appear and not experience any of the other overt flu-like symptoms.
An Example of a Lyme Disease Journey
In the early spring of 2014, my step-son began to experience random swelling in one finger and then another. At the time he was a competitive weightlifter so he assumed it was a soft tissue injury. When his toes started to swell, he realized that this symptom could not simply be the result of lifting weights. By this point, he had also started to experience a strange rash on the palms of his hands and souls of his feet that peeled continuously. After several appointments with his family doctor over a period of 10 months, a referral was made to a Rheumatologist which lead to a diagnosis of Psoriatic Arthritis (a form of arthritis that includes symptoms of psoriasis) in June 2019. When asked about the underlying cause of PA, the Rheumatologist stated it was "just bad luck", claiming the causes were unknown. This answer wasn't acceptable to us so we started to investigate other underlying causes.
We started to suspect that his PA might have something to do with Lyme Disease caused by an undetected bite in the Spring of 2014. We came to this conclusion as my step-son was bitten and treated for a tick bite in April 2015. Initially, he felt mild symptoms of fatigue and nausea, but a tell-tale Lyme Disease bullseye rash appeared at the location of the tick bite 5 days later. When the rash appeared, I took him to the hospital and he was given a short course of antibiotics to 'prevent' Lyme Disease. He noticed that while on the antibiotic, the pain and swelling in his hands reduced.
When the Rheumatologist declared a diagnosis of PA he prescribed Methotrexate, (an immunity-suppressing drug). Given the serious nature of the drug and our suspicions of Lyme Disease, my step-son declined the prescription and his mom asked the Rheumatologist for a Lyme Disease test. Initially, the doctor was reluctant to have the test performed as he didn't see any connection to Lyme Disease and PA. After further discussion, he agreed to order the test and much to the doctor's surprise, it came back positive.
Unfortunately, the Rheumatologist still held to his original recommendation of Methotrexate while my step-son was being treated for Lyme. This recommendation was declined but it demonstrated a disturbing lack of information about Lyme Disease and the integration of the various arms of the medical system. The treatment for Lyme Disease should not include the active suppression of the immune system.
As of October 2015, my step-son was being actively treated for Lyme Disease with allopathic medicine and holistic supports (they're listed below).
As of April 2017, he was still experiencing symptoms of swelling and pain in two of his fingers, was no longer on allopathic medication and continues holistic supports.
Since 2018 he has gone through two surgeries. One to remove chronically infected tonsils and the other, an emergency appendectomy. His naturopathic doctor speculated that the infection in his tonsils could be contributing to his lingering symptoms as they might have been harbouring Lyme Disease. Once they were removed, his symptoms did reduce. Was this from an ongoing Lyme or another co-infection? We do not have definite proof but it is worth noting.
I also speculate that his appendix might have been compromised by the disease. Contrary to popular belief, the appendix does serve important functions in the body. One function is to house and repopulate the bowel with friendly and vital gut bacteria that make up our microbiome. When our healthy gut bacteria is too low, the appendix expresses the much-needed microbes into the colon.
How long does a tick need to be on the body to transfer Lyme?
The Centers for Disease Control (CDC) suggests that a tick must be attached to your body for at least 36 hours to transmit Lyme Disease. Unfortunately, the information from the International Lyme and Associated Disease Society website states differently, "While the longer the tick is attached, the higher the risk of transmission, it is possible to get Lyme Disease even if the tick is attached for less than 24 hours. The salivary juices of the tick, which contain anticoagulants, anesthetics, and immune suppressors, also contain microbes that can be injected at the time of attachment. Transmission of bacteria by ticks attached less than 24 hours has been well documented in animals, and a recent paper ... documented that this can occur in humans as well."
This was the case for my step-son. The tick he had on his body in April 2015 was only there for a few hours, yet he still developed the classic bullseye rash at the site of the bite. It's important to remember that although transmission cannot occur without the tick bite, up to 50% of people may not remember being bitten because the deer tick is tiny, and its bite is usually painless. The scariest thing is that a tick can be as small as the period at the end of this sentence.
If you have symptoms of Lyme Disease without the distinctive rash, your doctor will need to rely on questions such as “Have you have been outdoors in an area where Lyme Disease is common?” and “Do you remember being bitten by a tick?” Your doctor should perform a physical exam and run laboratory tests to check for the presence of antibodies to B. burgdorferi to help provide a diagnosis. Unfortunately, the tests used are not always accurate.
According to the Canadian Lyme Disease Foundation
“The Myth… I was tested for Lyme Disease at the provincial lab, and the results were negative. I guess that means I can't have Lyme.
The Truth… Actually, that’s untrue. Evidence suggests that Canada’s Lyme testing methods are flawed. False-negative test results are common, especially in the early stages of Lyme. It takes time for antibodies to develop, so early tests often miss the bacteria. Contrary to bureaucratic statements, late-stage Lyme Disease antibody testing is much less accurate.
Testing for Lyme Disease can be very challenging – in fact, many patients receive several false negatives before being correctly diagnosed. To avoid misdiagnosis, it’s critical that you identify your symptoms and are tested by a doctor as soon as possible.
Why Lyme is tough to diagnose?
- Lyme symptoms are similar to other illnesses, so misdiagnosis is common.
- Many Canadian doctors are unfamiliar with Lyme, so they don’t test for it or administer the wrong tests.
- Only a handful of blood tests effectively detect Lyme bacteria, so the infection is often missed.
Don’t get discouraged if you get a negative diagnosis. Seek out second, and even third, opinions if you must!”
Co-Infections & Chronic Lyme Disease
Once infected with B. burgdorferi, It will take a few weeks to produce antibodies against the bacteria. Unfortunately, this can lead to a delay in treatment. Patient advocate groups suggest that this delay can increase symptoms and make the disease more difficult to treat.
Additionally, there are co-infections that can occur that complicate treatment. Patient advocate groups, and some medical experts, now believe that those with these co-infections often don’t respond well to the usual treatments. It may take an experienced doctor to properly identify and treat each tick-borne infection. Co-infection generally results in more severe illness and longer recovery time. If you feel you may have Lyme Disease, you can take the
Horowitz Lyme MSIDS Questionaire by clicking here. This does not replace medical diagnosis and treatment, but it gives you more information to work with.
Though it's anecdotal, I know several people who are dealing with what is now being called ‘Chronic Lyme Disease.’ This topic is very controversial, so I recommend reviewing the following websites for more information :
Lyme Disease misdiagnosis
It is now starting to be understood that many Lyme victims are commonly misdiagnosed with other illnesses. This is both frustrating and dangerous for the person afflicted with this disease. It means that treatment can be either delayed or incorrect. The following chart was taken from the
Canadian Lyme Disease Foundation website.
If you have a sudden onset of one of these conditions and live or visited an area where ticks are present, you may consider being tested for Lyme Disease. I would add type Latent Autoimmune Diabetes in Adults (LADA) to this list. This is also unofficially known as type 1.5 Diabetes.
In the USA, doctors that have experience diagnosing and treating Lyme Disease frequently use one of two antibody tests as a first-level screening: the ELISA and Western Bot. According to Lyme Disease expert, Stephen Harrod Buhner, these two tests can only detect 60% of those with Lyme Disease. Unfortunately, the other tests available (such as PCR, CXCL13 and CD57) are not much better. Apparently,
"...the 'Advanced Laboratory Lyme' test is averaging a 92 percent accuracy for diagnosing Lyme infection. The downside is that it takes two to four months. For long-standing Lyme infections have refused to be diagnosed through other testing methods, this might be a good choice." For more information about the work of Stephen Harrod Buhner,
click here.
If you are experiencing ongoing symptoms, despite a negative Lyme Disease test result, it is important to continue to seek help. Whether you have Lyme Disease or not, you should not let your symptoms be left undiagnosed, and therefore, untreated. The International Lyme and Associated Diseases Society (ILADS) is an international resource that continues to update information on Lyme Disease.
Check out their website for more information.
Treatment for Lyme Disease
Antibiotics are prescribed to treat Lyme Disease to help speed healing of the bullseye rash and keep symptoms, such as arthritis and nervous system problems, from developing. In general, it is thought that the sooner treatment begins, the quicker and more complete the recovery.
I have been asked if Lyme Disease can be treated without the use of antibiotics. At one point, I would have said, "Given the nature and severity of this disease, this is one of those cases where I feel grateful to have a medical treatment that works in some cases."
Now I am not so sure. The antibiotic treatment does not work in ALL cases, and it appears in some circumstances, the antibiotics only kill off the weaker bacteria and force the stronger ones into hiding. This might have to do with how quickly the antibiotics are used, and if the treatment is thorough enough. I believe it is very important to follow-up allopathic treatment with other holistic supports, as described in the section below.
After receiving treatment for Lyme Disease, patients may still experience muscle or joint pain and symptoms that relate to the nervous system, such as trouble with memory and concentration. Researchers continue to investigate the ideal length for a course of antibiotics for the various symptoms that can result from Lyme Disease. I, personally, know two people who are on long-term antibiotic treatments for arthritic symptoms arising from confirmed cases of Lyme Disease. When they stop the antibiotics, the arthritic symptoms return. Having Lyme Disease does not make you immune to reinfection; individuals previously infected and diagnosed with Lyme Disease can be infected again if bitten by an infected tick.
Another example of a Lyme Disease Journey
In June 2014, my son Taevan was treated for Lyme Disease. He does not remember being bitten by a tick, so his initial symptoms were undiagnosed. Unlike his step-brother, his symptoms were severe. He experienced a temperature of 105oF, body aches, chills, disorientation, nausea, mind-numbing migraines, profound joint pain, sensitivity to light, lack of coordination, vertigo, stiff neck, Bell’s palsy (paralysis of one side of his face) and extreme fatigue. He could barely move! Meningitis was ruled out fairly quickly, and our whole family was so frightened because we had no idea what was going on.
Five days and three trips to the hospital later, a large bullseye rash appeared on his leg. It was a huge relief to find out what it was. Unfortunately, dealing with two different doctors at the hospital led to a discrepancy in diagnosis – even after the bullseye rash appeared.
Given the severity of his symptoms, I advocated for my son to be treated for Lyme Disease with allopathic treatment, and he was placed on the oral antibiotic Teva-Doxycycline. Within 24-hours, his fever started to diminish and his symptoms calmed a bit. It took two months before he felt he was on the road to recovery, though he was well on his way to feeling better within 72-hours. In this case, I believe the antibiotics were a very useful and important tool in quickly addressing the infection.
A couple of days after the antibiotic treatment began, my son underwent testing for Lyme Disease. We waited for two months to get the results and they came back negative. Fortunately, he didn't need to wait that long for treatment!
Holistic support for treating Lyme Disease
As soon as my son began antibiotic treatment for Lyme Disease, I started to support him with supplements and holistic therapists (chiropractor, osteopath, acupuncturist and massage therapist). Because of my extensive investigation and research into Lyme Disease, I pulled out all the stops. I was aware that Lyme Disease could take its toll as I knew many other people in the Ottawa Valley of Ontario, Canada had been profoundly affected by the condition. Unfortunately, we live at ground zero for Lyme Disease for Ontario, Canada. This was something that took a long time for our community figure out. As a result, every household I know in our community has felt the impact.
Below is a list of the holistic supports I used to treat my son's symptoms. I provide this list for information only. It is not meant as a recommendation for treatment. Please do your own investigative work and discuss these treatments with your Naturopathic Doctor or Holistic Medical Doctor before using them.
- Strict no-sugar, no-grain, Paleo-Keto Diet to deny the disease anything to live on! (Consider the delicious protocol laid in Julie's book, Hot Detox.) My son needed to remove all sweeteners and remain on a low carbohydrate protocol for an extended period of time.
- Celt Immuno-Care – To support the immune system.
- 100 Billion Probiotic – Taken away from an antibiotic. (My son used Genestra HMF Forte. Not everyone responses the same way to a probiotic. It can take a bit of experimentation to figure out which one is most effective.)
- AlliMax Garlic – This helps to kill stubborn infections and parasites.
- Wobenzyme – It helps to break down the bacteria biofilm that protects the microbe.
- MS+ – It helps heal the tight junctures in the bowel and prevent leaky gut.
- Digestive Enzyme – These help to digest food when the digestive system is compromised.
- Curcumin Active by AOR – This helps to reduce inflammation.
- NutraSea HP – This helps to support the nervous system, bowel, joints and brain function.
- Lyme Ease by Harmonic Arts – This formula helps to support the immune system with Cat's Claw, Andrographis, Smilax, Ashwagandha, Teasel Root and Japanese Knotweed. Some practitioners suggest taking these herbs separately as the dose of each herb might need to be adjusted according to the person's needs.
- St. John’s Wort 350mg – This helps support and repair the nervous system.
- Advanced B Complex by AOR – This helps support and repair the nervous system.
- Ortho-Adapt by AOR – This helps support and repair the nervous system.
- B6 100mg – Again, this helps support and repair the nervous system.
- Zinc Citrate 30mg – This helps to support the immune system.
- Liposomal Lypo-Spheric Vitamin C – This helps to support the immune system.
- Tissue Salt: Magnesia Phosphorica
- Tissue Salt: Ferrum Phosphoricum
- Tissue Salt: Kali Phosphoricum
- Homeopathic Aconitum Napellus 30CH
- Homeopathic Ledum Palustre 1M (Speak to your ND, Homeopath or Holistic Medical Doctor when using a homeopathic remedy at this dose.)
- Acupuncture, chiropractic, massage and osteopathic treatments.
After the antibiotics were done, and most of the symptoms were gone, my son continued to use many of these holistic supports for 12 months. If you've had digestive issues before being diagnosed with Lyme Disease, talk to your ND or Holistic MD about continuing these supports until all symptoms of your digestive disorder are gone and your bowel and digestive function are normal. This may require another healing protocol from a health practitioner.
Another important part of Taevan's lifestyle is the work of Wim Hof. Taevan practices the techniques taught by Wim Hof every day and feels it contributes to his physical, mental and emotional health. For more information on Wim Hof,
click here.
From my experience with clients with Lyme Disease, a full recovery depends on the health of the bowel, which is a large part of the immune system. Unfortunately, repeated use of antibiotics can cause gut dysbiosis, which requires a long-term strategy to heal. Consider reading Julie's book,
Hot Detox, for more information on digestive health and all of the detoxification systems of your body.
The presence of black mould can contribute to Chronic Lyme. Check your house (especially your basement) for evidence of black mould. It is necessary to have it removed completely by a mould specialist. DO NOT ATTEMPT TO REMOVE IT YOURSELF. Treating mould with bleach does little to kill it and it can expose you to a health-threatening dose of the spores. Speak to your ND, Homeopath or Holistic Medical Doctor about internal treatments.
The good news is that my son was able to make a full recovery. The combined effort of diet, supplements, alternative physical therapies, the Wim Hof technique and early medical treatment all contributed to a positive outcome. This is why I feel it's important to share all this information with you. Had we known what my step-son was dealing with, we might have been able to start treating him much sooner.
And the journey continues...
I wish I could say that our family's journey with Lyme Disease ended there. While on a trip to Australia in 2011 to visit my husband's family, we went on a bushwalk in a dense jungle area. The walk was amazing, but we brought back more than memories. While showering hours after the hike, I looked down to discover my abdomen was covered with tiny ticks that had latched on. I yelled to my husband, Jeff, and we started to do our first official tick check! We both had them all through our hair and down our bodies. Three of the tick on me were so imbedded I had to go to a walk-in clinic to have puncture hole biopsies done to remove them. Two of these ticks were on my butt! We had to fly home the next day and needless to say, my 36-hour transit back to Ontario, Canada was not pleasant.
Over the next few years, Jeff started to slowly experience symptoms that were not responding to holistic supports. He developed rosacea, arthritic pains in his hands and gout in his feet. He altered his diet by adding and taking away various foods. Nothing appeared to be resolving his symptoms, but he did notice that if he ate any animal protein, his face would become so inflamed, it felt like he has been burnt by acid. A series of hives would appear on his forehead that would later resolve to patches of dry skin that looked like he had been sunburnt. He removed meat, poultry and fish, which helped a bit, but overall his arthritic symptoms persisted.
In 2016, while Jeff's brother was visiting from Australia, he alerted us to a condition that had been linked to a Lyme disease. It appeared to cause an 'allergy' to meat (5) and one of the symptoms was urticarial. Considering our sons' histories with Lyme, Jeff decided to follow a similar protocol, and sure enough, his symptoms of urticarial, rosacea, arthritis and gout reduced dramatically. Note: Jeff was not tested for Lyme, so we do not have proof he had the condition. He did speak to his doctor before deciding to use holistic supports instead of antibiotics.
My best tips for preventing Lyme Disease
The best way to prevent Lyme Disease is to avoid contact with ticks. Given the amount of amazing green space we have in North America, this can be a bit of an issue. Incidents of Lyme Disease in North America appear to be concentrated in Eastern Canada, Manitoba and Eastern United States... just know that it can and does occur everywhere! Plus, though not as common in the cold winter months, tick bites can occur year-round.
Pregnant women, in particular, should avoid ticks in known Lyme Disease areas as infection may be transmitted to the fetus.
According to Lyme Disease expert, Stephen Harrod Buhner, the "Borrelia spirochetes are present in a variety of other biting arthropods, such as mosquitos, mites, fleas and biting flies and transmission through some of these routes have been documented." (1) It is important to take precautions when dealing with any type of insect bite.
I don’t want you to become frightened about being in nature! Communing with nature is a very important part of being healthy.
Useful tips for avoiding ticks and tick bites
- GO LONG! Wear long pants, long sleeves and long socks to keep ticks off your skin. Make your health and fashion statement! Tuck your shirt into your pants, and your pant legs into your socks or shoes to keep ticks (and other insects) on the surface of your clothing. If outside for a long period of time, tape the area where pants and socks meet to prevent ticks from crawling under clothing. Wear light-coloured clothing to make it easier spotting ticks.
- BE SITE SMART! Unless you are prepared, avoid wooded areas and nearby shady grasslands. Ticks and other insects are common in these areas, and particularly common where the two areas meet. Maintain a clear backyard by removing yard litter and excess brush that could attract deer and rodents. Maximize the sunlight in your backyard.
- TICK CHECK! Once indoors after being outside, check for ticks using a bright light, especially in the hairy areas of your body (including the groin, genitals and head) and place your clothing into a hot dryer for 15 minutes to kill any ticks that you have brought home with you. (Washing your clothes will not kill a tick!) Ideally, having a Tick Check Partner to help you with the tick-check process is the best option. Before letting pets indoors, check them for ticks. Ticks often fall off pets and then attach to humans. Plus, pets can also develop Lyme Disease.
- HAIL CEDAR! Consider using Cedar Essential Oil around your porch area and places where adults, children and pets frequently walk and play. Cedar oil kills ticks in all life stages and is safe for humans, animals and the environment. This US company has a pre-made kit you can use on your yard, while this Canadian company sells Cedar Essential Oil in larger quantities. Make up your own spray by diluting the oil in water prior to spraying with a yard hose-end sprayer.
How to make Natural Tick Repellent (aka Natural Phylum Arthropoda-Repelling Perfume)
There has been much controversy about claims that natural essential oils can protect you from insect bites, so I will not be debating that claim here. Instead, I invite you to try out a perfume mixture before heading out to party in nature. Be sure to source your essential oils from a very high-quality essential oil company. Low-quality brands will require more drops to make this recipe and may contain artificial scent enhancers that are unhealthy.
Essential oils have been used for thousands of years to adorn the body with pleasant aromas.
In a spray bottle, combine:
- 500 mL of Witch Hazel
- 10 drops of organic Cedar essential oil
- 10 drops of organic Rose Geranium essential oil
- 10 drops of organic Citronella essential oil
- 10 drops of organic Camphor essential oil
- 10 drops of organic Rosemary essential oil
Shake well before applying. Do not get it in your eyes! Be cautious when using any new product on a child.
Tick Bite! How to remove a tick
What we do know id that your risk of infection can be decreased by promptly removing ticks.
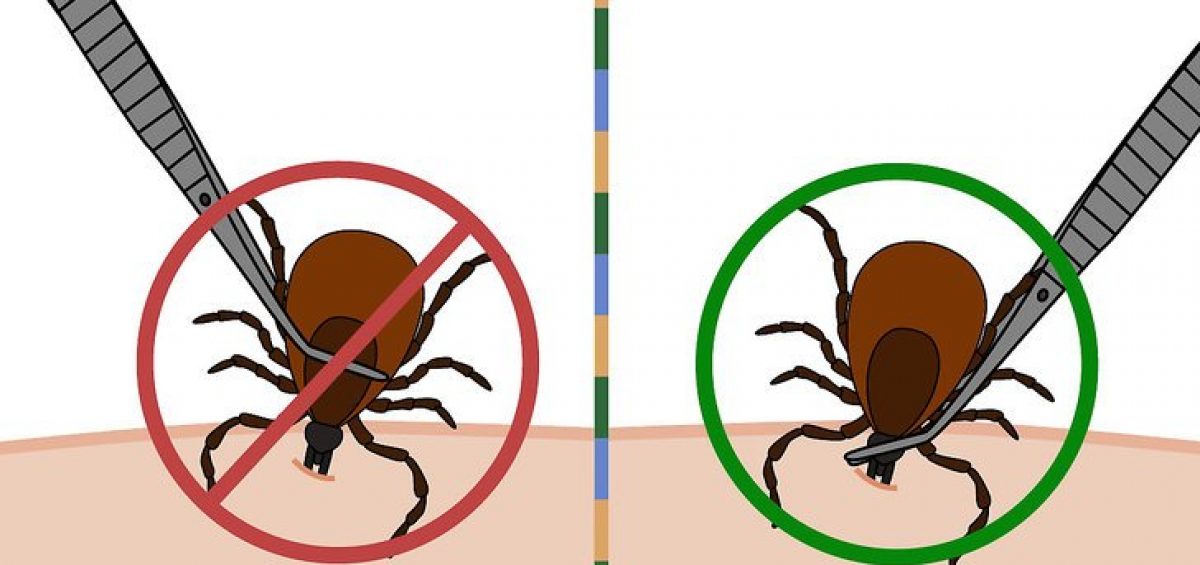
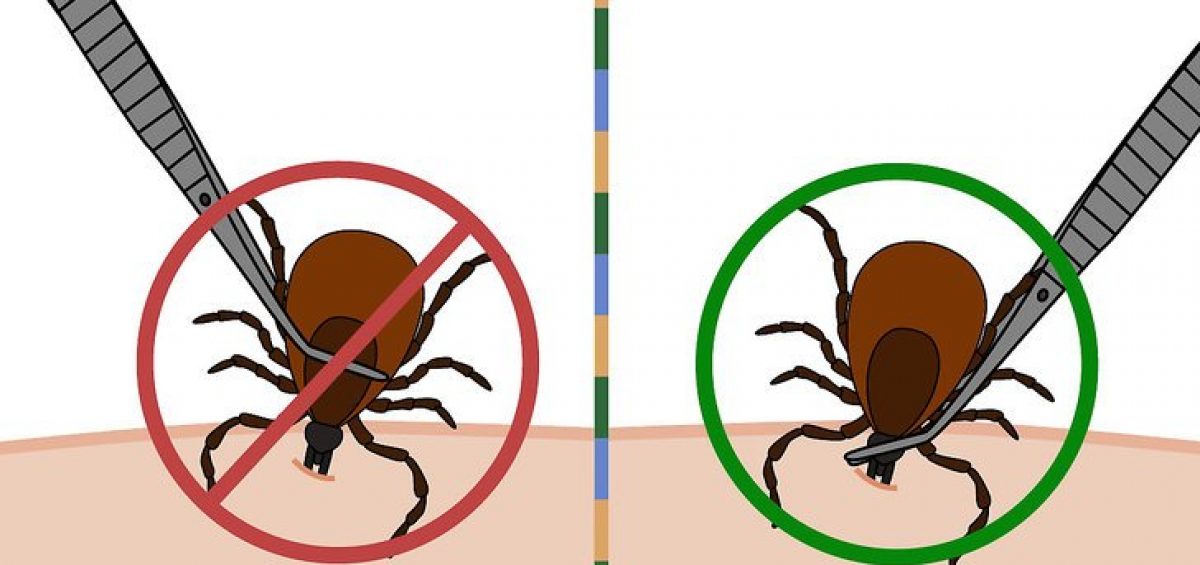
1. If you do get a tick bite, remove it using fine-tipped tweezers and – whatever you do – remain calm!
- Do not use petroleum jelly, a hot match, nail polish, essential oils or other products, as these techniques will NOT effectively remove the tick.
- Again, according to the ILADS website: "Any manhandling of the tick such as squeezing it, putting Vaseline over it, or holding a hot match to it, will increase the chance of transmitting bugs."
2. Grab the tick as close to the head as possible and pull it out gently so that ALL parts of the tick are removed.
3. Be careful not to crush the body of the tick as this can cause it to inject bacteria into your body.
4. Wash your hands with soap and water and clean the bitten area with an antiseptic or soap and water.
5. Place the tick in a tightly closed container for examination by your local health department or healthcare provider.
6. Contact your doctor about possible prophylactic treatment if your area is known to have Lyme Disease and/or if you have a compromised or suppressed immune system and/or if you were unable to remove the entire tick.
 Note:
Note: There are many Health Departments in Canada and the USA that no longer accept ticks for analysis. It's still a good idea to keep the tick, sealed in a container, in case you develop symptoms.
Final thoughts
Upon hearing the impact that Lyme Disease can have on someone's life, many people become frightened of going outside and interacting with the natural world. In no way am I attempting to alarm you with this information. Rather I strive to arm you with research, experience and alternatives that you can bring to your own health care practitioners. I love the outdoors. My hikes through the forest are an intricate part of my daily life. I encourage you to pay attention to nature and develop an intimate relationship with it, so you too can enjoy your time in the wild.
References
- Healing Lyme: Natural Healing of Lyme Borreliosis and the Coinfections Chlamydia and Spotted Fever Rickettsiosis, 2nd Edition by Stephen Harrod Buhner, 2015
- Natural Treatments for Lyme Coinfections: Anaplasma, Babesia, and Ehrlichia by Stephen Harrod Buhner, 2015
- Health hazards of mosquito repellents and safe alternatives: V.P. Sharma, National Institute of Science Technology and Development Studies: Current Science, Vol 80, No3 February 2001
- DDT Exposure in Utero and Breast Cancer: Barbara A. Cohn, Michele La Merrill, Nickilou Y. Krigbaum, Gregory Yeh, June-Soo Park, Lauren Zimmermann, and Piera M. Cirillo: The Journal of Clinical Endocrinology & Metabolism June 16, 2015
- Tick bites and red meat allergy: Commins SP, Platts-Mills TA. Curr Opin Allergy Clin Immunol. 2013 Aug;13(4):354-9. doi: 10.1097/ACI.0b013e3283624560. PMID: 23743512; PMCID: PMC4235259.







 Note: There are many Health Departments in Canada and the USA that no longer accept ticks for analysis. It's still a good idea to keep the tick, sealed in a container, in case you develop symptoms.
Note: There are many Health Departments in Canada and the USA that no longer accept ticks for analysis. It's still a good idea to keep the tick, sealed in a container, in case you develop symptoms.
